CBS News
When a teenager’s heart stopped, his friends jumped into action — and their CPR training saved his life

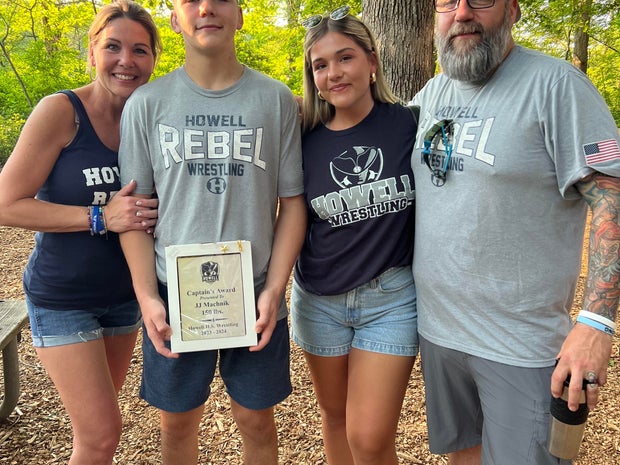
May 10 started like any other day for Laura Machnik, who said good-bye to her 18-year-old son J.J. before she headed to work. He was headed to work out at a friend’s house that morning, and after she arrived at work, Machnik confirmed that he had made it there safely.
Just minutes later, her phone rang. It was the mother of the friend J.J. was visiting, calling with news Machnik had been dreading for years.
At 14, J.J. had been diagnosed with hypertrophic cardiomyopathy, a genetic heart disorder that can cause sudden cardiac arrests. He was an active athlete and never had other symptoms of the disease, like shortness of breath or chest pains. But shortly after beginning his workout alongside friends Trevor Hodgins, 14, and Giovanni Scafidi, 18, his heart stopped.
“(She) called me and said ‘You have to get to my house as fast as you can, J.J. passed out on the treadmill,'” Machnik told CBS News. “All I said was, ‘Does he have a pulse?’ as I was running out the door from work … knowing what was going on, I’m just like, ‘OK, this is for real. This is it.'”
As Machnik drove over, Hodgins and Scafidi jumped into action, providing CPR and calling 911. When the first responders arrived, Hodgins and Scafidi told paramedics about J.J.’s diagnosis, so they could treat him immediately. His friends’ rapid response and quick thinking helped save J.J.’s life, his longtime cardiologist said.
Laura Machnik
“They gave him the best chance to survive,” said Dr. Matthew Martinez, a sports cardiologist and expert in hypertrophic cardiomyopathy at Morristown Medical Center in New Jersey. “They told me it was less than a minute before they started CPR. Those are the phrases we really want to hear when we’re looking for how kids are going to do after an event like this.”
What is hypertrophic cardiomyopathy?
Hypertrophic cardiomyopathy is a genetic heart disorder, affecting about 1 in 500 people, according to Martinez. The disease causes the heart muscle to become abnormally thick, which makes the heart inefficient at pumping blood.
There are two subgenres of the illness: obstructive and non-obstructive hypertrophic cardiomyopathy. J.J. was diagnosed with non-obstructive hypertrophic cardiomyopathy, which affects about a third of all patients. This version of the condition makes it possible for the heart’s left ventricle to stiffen, but does not stop blood from flowing like obstructive hypertrophic cardiomyopathy can.
Martinez said that children are usually tested for the condition if a parent is known to have it — and J.J.’s father, Jeff, had been diagnosed with the condition a few years before. J.J. was tested for it at age 14 after a routine checkup returned abnormal test results.
Laura Machnik
Symptoms of hypertrophic cardiomyopathy include chest pain and difficulty breathing, according to the Cleveland Clinic’s website. Monitoring and treating the condition is largely about measuring those symptoms and the impact they’re having on a patient’s life, Martinez said.
For J.J., an athlete and active teenager, that meant annual checkups and carefully considering what sports he would participate in. It also meant making sure the people around him knew what to do if he experienced a sudden cardiac arrest.
“We would talk about how you can make sure that you remember, and your coaches remember, that low risk doesn’t mean no risk,” Martinez said. “We prepared for that. We talked about CPR with his mom and dad. We made sure that coaches knew, that the high school knew, and he went and bought his own automated external defbrillator.”
J.J. also made sure that his peers and teammates knew how to do CPR. That training helped keep him alive when he collapsed in May.
“J.J. is alive because his friends acted quickly, because we had prepared for this,” Martinez said.
Treating sudden cardiac arrest
On the way to the hospital, J.J. coded twice in the ambulance and had to be resuscitated by paramedics. After he was stabilized, he was transferred to Morristown Medical Center. There, he was met by cardiologist Dr. Amirali Masoumi, and several days of intense treatment began.
The situation was “rather complicated,” Masoumi said. His heart, which normally pumps at about 70% of a standard person’s function, was only working at a rate of about 20%, Martinez said.
J.J. was placed in an induced coma, and his body was cooled to preserve as much brain function as possible. Over the next 24 hours, his kidney function also began to decline, and his heart continued to have trouble beating. This led Masoumi to put J.J. on an ECMO, or heart-lung, machine to let his organs rest. The whole time, no one knew how much J.J.’s brain function would be affected, Masoumi said, which made the care even more complicated.
“We gathered, we had a very honest conversation with the family, a harsh, tough conversation, telling them that if he doesn’t wake up, if the brain doesn’t show any signs of recovery, it doesn’t matter how many machines we have, it doesn’t matter if we resuscitate the heart and lungs, unfortunately our options will be limited,” Masoumi said. Three days after his collapse, on Mother’s Day, the family had a candid conversation about the possible need for a heart transplant if J.J. woke up.
“J.J. is an envelope pusher,” his mother said. “The night before, heart transplant was on the table. That’s how we went to bed. … Then we wake up and his heart started working. It just started working again. I said, ‘Could it be any other way than the J.J. way, to hear the worst possible information and then say ‘Oh wait, just kidding, here I am?’ That is our son.”
By early morning on May 14, there were still only limited signs of brain function, Masoumi said. But just hours later, J.J.’s condition took a turn for the better.
“I really didn’t expect from like, 6:30 in the morning to 9, that he would perk up and start fighting,” said Masoumi. “It was extremely rewarding to hear that. The rest is easy, because now we’re in a game we know. We know the heart. The brain is intact. He was following commands. We knew that we would have options for him.”
Laura Machnik
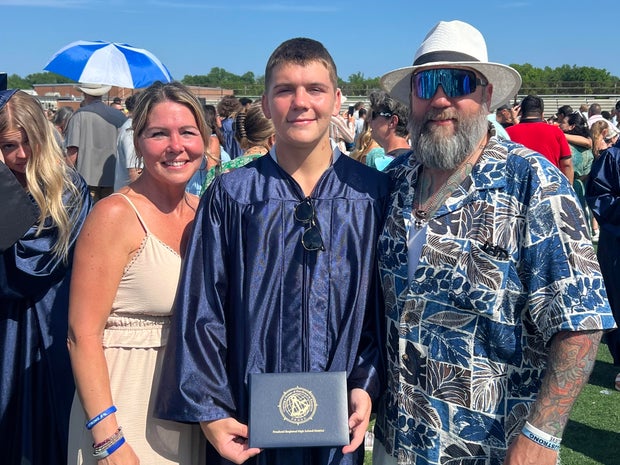
On May 17, J.J. celebrated his 19th birthday with some walking and beginning physical and occupational therapy. On May 23, he was discharged from the hospital, less than two weeks after he was admitted. Now, he has an internal cardiac defibrillator implanted in his chest, which will hopefully avoid future sudden cardiac arrests, Martinez said.
He will continue to be monitored regularly, Martinez said. For now, athletics are off the table, but Machnik said J.J. has thrown himself into end-of-year activities like prom and his senior picnic. On June 20, he walked across the stage at his high school graduation.
Just days beforehand, he told CBS News that he was looking forward to the day and celebrating how far he had come since the sudden cardiac arrest just a month before.
“After what happened, which was devastating, it’s been the best it can be,” J.J. told CBS News.
Laura Machnik
CBS News
A study to devise nutritional guidance just for you

It’s been said the best meals come from the heart, not from a recipe book. But at this USDA kitchen, there’s no pinch of this, dash of that, no dollops or smidgens of anything. Here, nutritionists in white coats painstakingly measure every single ingredient, down to the tenth of a gram.
Sheryn Stover is expected to eat every crumb of her pizza; any tiny morsels she does miss go back to the kitchen, where they’re scrutinized like evidence of some dietary crime.
Stover (or participant #8180, as she’s known) is one of some 10,000 volunteers enrolled in a $170 million nutrition study run by the National Institutes of Health. “At 78, not many people get to do studies that are going to affect a great amount of people, and I thought this was a great opportunity to do that,” she said.
CBS News
It’s called the Nutrition for Precision Health Study. “When I tell people about the study, the reaction usually is, ‘Oh, that’s so cool, can I do it?'” said coordinator Holly Nicastro.
She explained just what “precise” precisely means: “Precision nutrition means tailoring nutrition or dietary guidance to the individual.”
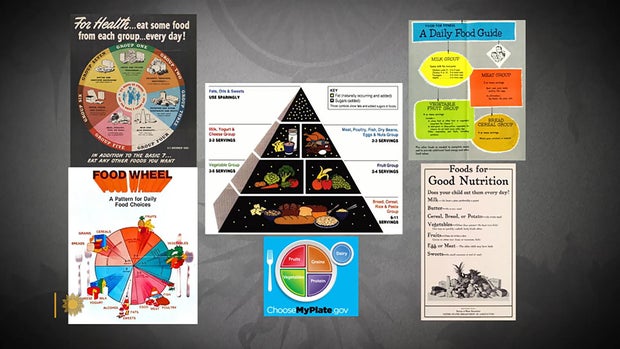
The government has long offered guidelines to help us eat better. In the 1940s we had the “Basic 7.” In the ’50s, the “Basic 4.” We’ve had the “Food Wheel,” the “Food Pyramid,” and currently, “My Plate.”
CBS News
They’re all well-intentioned, except they’re all based on averages – what works best for most people, most of the time. But according to Nicastro, there is no one best way to eat. “We know from virtually every nutrition study ever conducted, we have inner individual variability,” she said. “That means we have some people that are going to respond, and some people that aren’t. There’s no one-size-fits-all.”
The study’s participants, like Stover, are all being drawn from another NIH study program called All Of Us, a massive undertaking to create a database of at least a million people who are volunteering everything from their electronic health records to their DNA. It was from that All of Us research that Stover discovered she has the gene that makes some foods taste bitter, which could explain why she ate more of one kind of food than another.
Professor Sai Das, who oversees the study at Tufts University, says the goal of precision nutrition is to drill down even deeper into those individual differences. “We’re moving away from just saying everybody go do this, to being able to say, ‘Okay, if you have X, Y and Z characteristics, then you’re more likely to respond to a diet, and somebody else that has A, B and C characteristics will be responding to the diet differently,'” Das said.
It’s a big commitment for Stover, who is one of 150 people being paid to live at a handful of test sites around the country for six weeks – two weeks at a time. It’s so precise she can’t even go for a walk without a dietary chaperone. “Well, you could stop and buy candy … God forbid, you can’t do that!” she laughed.
While she’s here, everything from her resting metabolic rate, her body fat percentage, her bone mineral content, even the microbes in her gut (digested by a machine that essentially is a smart toilet paper reading device) are being analyzed for how hers may differ from someone else’s.
Nicastro said, “We really think that what’s going on in your poop is going to tell us a lot of information about your health and how you respond to food.”
CBS News
Stover says she doesn’t mind, except for the odd sounds the machine makes. While she is a live-in participant, thousands of others are participating from their homes, where electronic wearables track all kinds of health data, including special glasses that record everything they eat, activated when someone starts chewing. Artificial intelligence can then be used to determine not only which foods the person is eating, but how many calories are consumed.
This study is expected to be wrapped up by 2027, and because of it, we may indeed know not only to eat more fruits and vegetables, but what combination of foods is really best for us. The question that even Holly Nicastro can’t answer is, will we listen? “You can lead a horse to water; you can’t make them drink,” she said. “We can tailor the interventions all day. But one hypothesis I have is that if the guidance is tailored to the individual, it’s going to make that individual more likely to follow it, because this is for me, this was designed for me.”
For more info:
Story produced by Mark Hudspeth. Editor: Ed Givnish.
“Sunday Morning” 2024 “Food Issue” recipe index
Delicious menu suggestions from top chefs, cookbook authors, food writers, restaurateurs, and the editors of Food & Wine magazine.
CBS News
A new generation of shopping cart, with GPS and AI

Watch CBS News
Be the first to know
Get browser notifications for breaking news, live events, and exclusive reporting.
CBS News
“All hands on deck” for Idaho’s annual potato harvest

Watch CBS News
Be the first to know
Get browser notifications for breaking news, live events, and exclusive reporting.