CBS News
Medicare’s new $2,000 prescription drug cap goes into effect Jan. 1. Here’s how it works.

Starting Jan. 1, millions of Americans who get their prescription drugs through Medicare could get a major financial break when a $2,000 out-of-pocket spending cap on medications goes into effect.
The yearly price cap has been in the works since President Joe Biden signed the Inflation Reduction Act into law in 2022, with that legislation including provisions tackling drug costs for seniors as well as other Americans. While some of those other rules have already kicked in, such as a $35 price cap on insulin for seniors, Medicare’s $2,000 drug cap will become effective starting next month.
The out-of-pocket cost cap could be a “game changer” for many seniors, Ryan Ramsey, the associate director of health coverage and benefits at the National Council on Aging (NCOA) told CBS MoneyWatch. In the first year of the cap, about 3.2 million Medicare recipients are likely to see lower costs due to the new rule, particularly seniors who take multiple medications or have high-cost prescriptions, according to an analysis from AARP.
Before the law, there was no out-of-pocket cap for Medicare’s Part D, the section that covers prescription drugs, which left seniors at risk of “significant financial burdens,” the AARP noted.
“Having a cap where somebody can know, ‘Hey, this is what my maximum out of pocket will be for my medication,’ that will be an enormous deal,” Ramsey noted.
Here’s what to know about the new Medicare prescription drug spending cap.
Who is covered by the new Medicare drug cap?
The new $2,000 out-of-pocket cap on prescription drugs covers everyone with a Medicare Part D plan, which is the section of Medicare that covers most pharmaceutical products. The annual new cap also includes people with drug plans through Medicare Advantage, which are health plans offered by private insurers.
There are more than 50 million older Americans who have either Part D or prescription plans through Medicare Advantage, according to health policy site KFF.
Will Medicare’s so-called “donut hole” still exist?
No, according to Medicare. “Because of the prescription drug law, the coverage gap ends on Dec. 31, 2024,” its website states.
The so-called “donut hole,” or coverage gap, has affected almost all prescription plans. In the current calendar year, seniors could enter the donut hole once they and their plans had spent more than $5,030 on drug costs, at which point they were on the hook for out-of-pocket drug costs until they hit $8,000 in spending. Catastrophic coverage would kick in above that amount and cover additional spending.
Which prescription drugs are covered by the Medicare cap?
The $2,000 cap includes all the prescriptions that are in a Medicare recipient’s Plan D formulary, or a plan’s list of covered drugs. That means that if a doctor prescribes a drug that’s not on your formulary, it won’t be covered by the $2,000 cap, potentially adding to your costs.
Medicare enrollees can ask their doctors to prescribe drugs that are covered on their formulary, Ramsey noted.
“What I advise, in a situation where you are prescribed a new prescription, take your formulary to the doctor’s office. Say it’s a drug pressure medication, and you can say, ‘Can you make sure you can prescribe something that’s on my plan?,'” he noted.
In other cases, such as for new medications or drugs for which there aren’t alternatives, Medicare enrollees can ask for a drug exception, which can be granted if deemed medically necessary, according to Medicare.
Because formularies can change their coverage each year, and people’s prescriptions can also vary over time, it’s important to check your Part D plan during open enrollment each year to ensure you’re in the best drug plan for your needs, Ramsey added. Open enrollment typically occurs between mid-October to early December.
Do I need to sign up for the $2,000 out-of-pocket cap?
No, the cap will automatically be applied to your Part D plan, and the plan will track your spending. Once you hit $2,000, the new cap will go into effect and cover your eligible drug costs beyond that amount.
What costs are covered in the $2,000 Medicare Part D spending cap?
The new measure will cover medications included in your formulary, as well as your deductible, copayments and coinsurance for drugs that qualify for the cap.
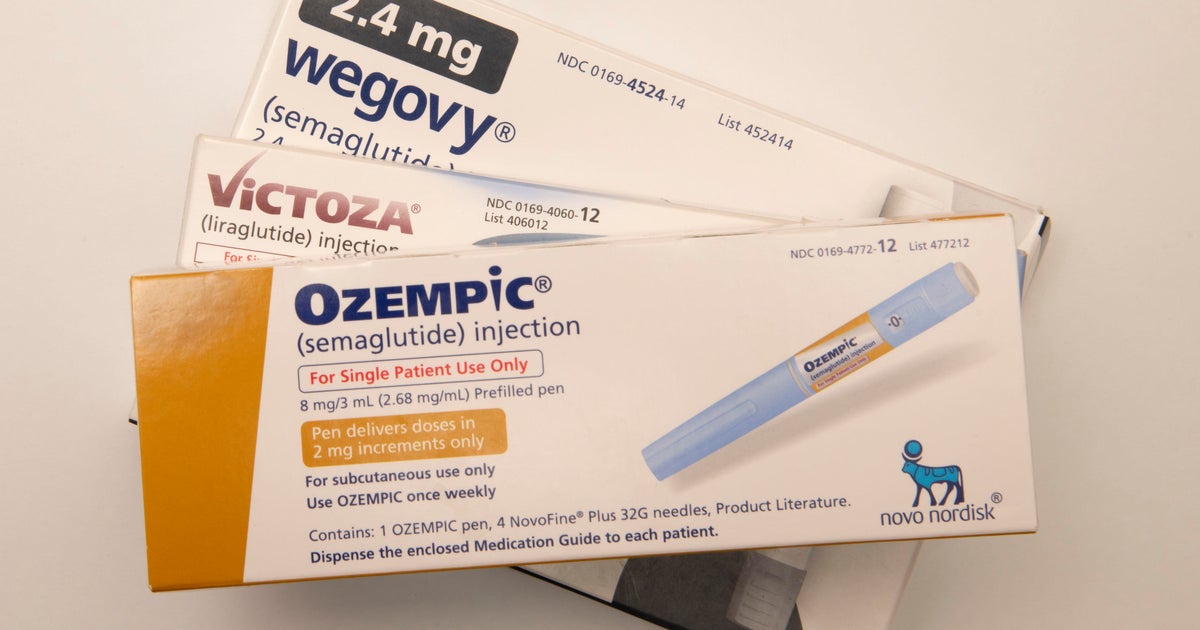
However, the cap doesn’t include coverage for drugs outside of your Part D plan, which means that it also doesn’t apply to pharmaceuticals covered by Medicare Part B, which include drugs you typically wouldn’t give to yourself, such as injectables that you’d get at a medical office.
It also doesn’t cover your Part D premiums.
The cap will allow people “to make better decisions on how to get their health care,” Ramsey noted. Prior to this change, “I have had discussions with people, ‘Am I going to buy groceries late in the year or pay for my prescriptions?'”
CBS News
IRS sending payments of up to $1,400 to 1 million people. Here’s who qualifies.

The IRS said Friday it is sending a total of $2.4 billion in “special payments” to 1 million people, part of an effort to ensure that Americans who didn’t receive all of their federal stimulus checks during the pandemic will get the money in their bank accounts.
The payments will vary by person, with a maximum amount of $1,400 per recipient, the agency said in a statement.
“To minimize headaches and get this money to eligible taxpayers, we’re making these payments automatic, meaning these people will not be required to go through the extensive process of filing an amended return to receive it,” IRS Commissioner Danny Werfel said in a statement.
Who will get a payment from the IRS?
The tax agency said it’s disbursing the funds after reviewing internal data that showed many people had filed tax returns but yet didn’t claim what is known as the “recovery rebate credit” in 2021.
That credit was designed for people who didn’t get all or some of the stimulus checks when they were issued during the pandemic. Lawmakers authorized three stimulus payments, with two sent in 2020 and a third in 2021.
Most taxpayers who were eligible for the stimulus payments have already received them directly, or later through the recovery rebate credit.
Do you need to apply for the IRS payment?
No. The IRS said it’s sending the payments automatically to about 1 million people who filed tax returns and who qualified for the recovery rebate credit yet didn’t claim it. The agency will send a letter to recipients to let them know they will receive the payment.
When will the IRS send the payments?
The tax agency said the checks will be sent in December, with most of the payments arriving by late January 2025.
The money will either be automatically direct deposited to the recipient’s bank account or will arrive in the mail via a paper check.
CBS News
Joy to the World | Sunday on 60 Minutes

Watch CBS News
Be the first to know
Get browser notifications for breaking news, live events, and exclusive reporting.
CBS News
Enter for a chance to win tickets to the Chicago Boat Show
Don’t miss one of the most amazing shows in the U.S. — Discover Boating’s Chicago Boat Show in partnership with Progressive Insurance. Enter now to win a 4-ticket-prize-pack to the event.
Read the original article